Contraception
Module created August 2019
Introduction
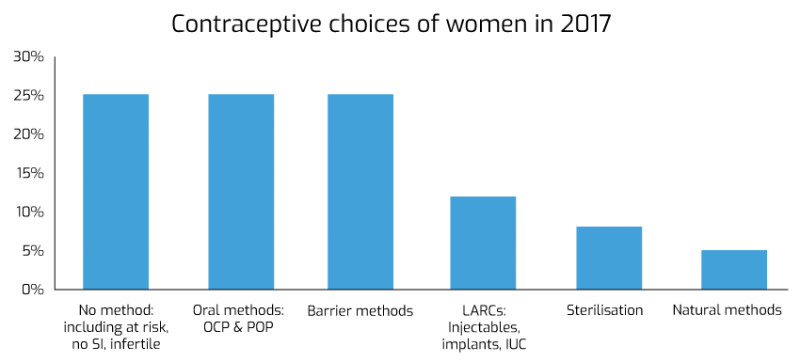
Contraception is a significant part of General Practice work. At any one time, up to 10% of women using contraception are dissatisfied with their current method. Over the last 60 years, contraception options have evolved unrecognisably. With the emergence of oral contraception in 1960s, shortly followed by intrauterine devices, progesterone only injectables and contraceptive implants, women in the 21st century have access to a variety of options, free under the NHS. Despite a recent push for long acting reversible contraception as the most cost-effective contraception, oral and barrier contraception are still the most prevalent (see figure 1). With no method being 100% risk free, choice will depend on medical eligibility, ease of use, side effect profile, as well as cultural influences in age, religion and community.
While many of these methods can be issued by sexual health clinics or pharmacies, a significant number of women will present to their GPs for contraception. With ever increasing options, it is important for GPs, and allied health care workers involved in contraception services, to keep up to date with best practice. This educational package aims to give an overview of contraception, based on the current guidance from FSRH (as of Summer 2019). It will cover oral contraception, progesterone only injectables, progesterone only implants, and intrauterine contraception. It does not cover emergency contraception, barrier methods, natural methods or sterilisation. For further details please visit FSRH website for a full and comprehensive list of guidelines.
This module was written by Dr Rebecca Ratcliffe GP in Cwmbran

