Physical Activity, Exercise and Immune Function
This section of this website, has been developed by healthcare professionals and scientists, in response to the Coronavirus infectious disease-19 (COVID-19) pandemic, and is written for healthcare professionals to enhance their understanding of how physical activity/exercise can support immune function and potentially minimise the severity of symptoms of COVID-19, if infected. It is one of a series of sections to increase their knowledge of physical activity and relevant to all individuals.
Section 1: Background to exercise immunology
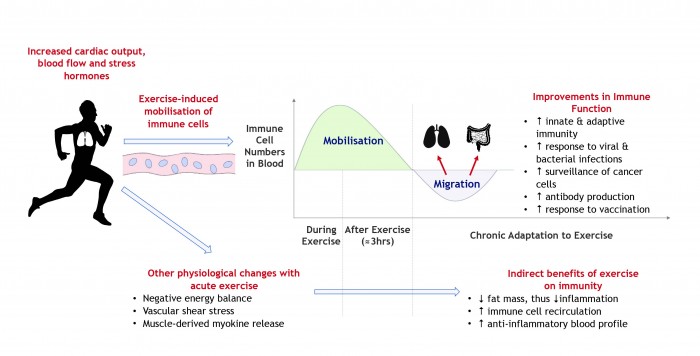
Researchers agree that regular bouts of moderate-to-vigorous intensity exercise (e.g. walking, running or cycling) can improve immune function and reduce systemic inflammation 1–3. The anti-inflammatory effects of exercise relate to changes in both body composition (i.e. lower central fat mass) and a steady summation of changes to the immune system after each session of exercise 4. Increases in cardiac output, blood flow and the release of stress hormones (e.g. adrenaline) during exercise result in immune cells with high functional capacity (i.e. neutrophils, natural killer cells and cytotoxic T-cells – see glossary) being mobilised into the bloodstream 5–7. These cells migrate from the circulation towards various tissues to survey the body for damage, infection and/or tumour cells 8. Each session of exercise therefore primes the immune system to ‘patrol’ the body and do its job effectively. Furthermore, the release of cytokines from muscle (termed myokines) induce an anti-inflammatory environment after each individual exercise bout 4,9,10. These exercise-induced changes to the immune system are an important consideration for healthcare professionals. Over the longer-term, engaging regularly in physical activity is also linked with a reduction in the number (≈ 40-50%) 11 and severity of infectious episodes (e.g. common cold and flu) individuals experience throughout the year 11,12. Collectively, over time, exercise can induce an array of benefits to the immune system (Figure 1) that optimise health and reduce the risk of infection and chronic disease.
Figure 1: Benefits of exercise on the immune system
Section 2: Can exercise suppress immune function?
Despite agreement by researchers that regular moderate-to-vigorous intensity exercise can improve host immunity, it is a very contentious issue as to whether arduous exercise (see box 1) can actually increase the risk of infection 3. This is of particular interest in the context of the current COVID-19 pandemic (section 3).
Traditionally, the J-shaped model of immunity has proposed that regular moderate intensity exercise can lower the risk of upper respiratory tract infections (≈60% of infections experienced), whereas a high volume of vigorous intensity exercise might increase this risk, relative to sedentary individuals 13. The evidence underpinning this model has been established from studies reporting a higher incidence of self-reported infections after competitive marathons 14 and heavy training periods in a variety of competitive team sports 15–17. Since then, some data have indicated that aspects of immunity are impaired after single 18–21, consecutive 22–24, and regular sessions (i.e. week/ months) 25–27 of arduous exercise (see box 1).
From the studies conducted, exercise volume (intensity x duration) of individual and consecutive sessions appears to be the key factor driving alterations in markers of immune function. It is believed that these alterations relate to the depletion of muscle glycogen and/ or depletion of energy reserves within immune cells, although these claims require further research to be substantiated 3,32. The points of contention on this topic are multiple, but primarily relate to disagreements over study design, validity of the biomarkers examined, appropriate diagnosis of infection and the immunological techniques used 3. It is important to emphasise that the data indicating that high volumes of training can causatively supress immunity need to be considered in the context of a range of other factors that can adversely affect immunity (see box 2) 33. The body cannot distinguish between these different types of stress, and many of these variables intertwine with exercise volume when ‘suppressing’ measures of immunity (e.g. stress induces cortisol release, which can suppress immune function). It is clear that heavy sessions of exercise, particularly if repeated over consecutive days, can dramatically alter markers of immune function 18–27; however, the evidence does not support a direct relationship between exercise load and an increased risk of infection. Indeed, a recent consensus statement from the International Olympic Committee suggests that elite athletes who effectively manage their behavioural (i.e. minimise pathogen exposure) and lifestyle habits (i.e. stress, sleep and nutrition) are not more likely to have a higher risk of infection, despite their very high training volumes 34.
A key take home message for the general population is that there is no evidence to indicate that engaging in vigorous intensity exercise within or even slightly over the recommended guidelines of 150 minutes per week is detrimental to immune function. On the contrary, regular engagement in moderate to vigorous physical activity and structured exercise is critical to stimulating the immune system to perform its job effectively.
Section 3: Staying active during the COVID-19 pandemic
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is the strain of coronavirus known to cause COVID-19, an infection of the lower respiratory tract that has caused widespread infection, morbidity and mortality worldwide. The government lockdown on March 23rd 2020 resulted in a new way of life for the British population. Isolation has confined individuals and families to their homes for prolonged periods, with restricted time outdoors. Emerging data from across the world are already indicating that lockdown resulted in reduced physical activity 35 and increased sedentary time 35,36. Even as lockdown restrictions ease, it is possible that these habits are maintained, which in conjunction with the stress of the situation could be detrimental to immune function and the risk of further developing chronic health conditions 37. Further, the likelihood of subsequent waves of infection may result in reinstatement of lockdown, so these forced lifestyle and habit changes may be ongoing.
Given that we are still in the infancy of what could be long-term changes to our way of life, there is time to alter daily activity and exercise habits to minimise the severity of symptoms of COVID-19, if infected. There are no empirical data to indicate that being more physically active or engaging in regular moderate-to-vigorous intensity exercise can directly reduce susceptibility to COVID-19 and/ or the severity of its symptoms. However, by building on the literature described in section 1, we can intuitively suggest potential benefits of regular moderate-to-vigorous exercise that can enhance immune function and could reduce the severity of COVID-19 symptoms and shorten recovery times (see box 3).
Section 4: Practical considerations for lockdown and beyond
Being more physically active and/or engaging in regular amounts of moderate-to-vigorous intensity exercise improves multiple aspects of immune function, which lowers one’s risks for infection and chronic diseases. Some specific considerations about daily activity and exercise are highlighted below:
- For more vulnerable population groups (older individuals and those shielding/ at a higher risk), home-based exercise is recommended to minimise pathogen exposure risk. Adherence to government guidance on social distancing and personal hygiene (hand washing and avoiding touching eyes, nose and mouth) are critical to minimise virus exposure.
- Any increase in physical activity is of benefit. While 150 minutes per week of moderate-to-vigorous intensity is a recommended target, regular bursts of exercise/activity for just a few minutes each day can benefit immune function and general health. Some examples include: walking around the garden, jogging on the spot, sit-to-stand exercises, or climbing the stairs in one’s house/apartment.
- If one is using this time to strive for personal performance goals by programming a high volume of training, they should pay special attention to their recovery time, nutrition, stress levels and sleep quality. Previous evidence allows us with some certainty to suggest that higher levels of aerobic fitness would likely reduce the severity of COVID-19 symptoms. However, it is conceivable that large volumes or large increases in training load could depress immune function, particularly if the variables outlined in Box 2 are not considered. It is a time to prioritise overall health and well-being, rather than performance.
Acknowledgments:
Motivate2move would like to thank Dr Alex Wadley and Dr Sam Lucas of the School of Sport, Exercise and Rehabilitation Sciences of the University of Birmingham, for their help in creating this section.
Planned review date July 2022
Physical Activity, Exercise and Immune Function - Factsheet - download
‘Strengthen your immunity’ - public leaflet
Now part of the RCGP clinical programme on physical activity and lifestyle
References: Can be found in Chapter 18
These factsheets are endorsed by the Royal College of General Practitioners (RCGP), British Association of Sport & Exercise Medicine (BASEM) and the Royal College of Nursing (RCN).




