Chapter 12 - Physical Activity and Respiratory Disease.
Asthma
Asthma is a common condition that affects people of all ages. Respiratory symptoms, such as intermittent recurrent dyspnoea and wheeze and variable expiratory airflow limitation are a result of increased airways hyper-responsiveness and airway inflammation.
Regular exercise is recommended as supplementary therapy to medication in people with stable asthma 1. The key benefits of exercise training in people with asthma are improved cardio-respiratory fitness and increased exercise capacity 1-3. In some individuals, regular exercise may also improve resting lung function 1, 3, asthma control and quality of life 1. While growing evidence suggests that obesity increases the risk of asthma 4,5, the benefits of weight loss for asthma control remain uncertain 6.
Exercise is well tolerated by people with stable asthma 2, 3. Nonetheless, exercise can pose a particular problem in some individuals, especially children, athletes and people with poorly controlled asthma, as exercise is a common trigger of asthma symptoms and bronchoconstriction. Symptoms and expiratory airflow limitation typically worsen after exercise, which varies in severity and implications depending on the severity of the disease, and this may also contribute to lower participation in physical activity 7.
To prevent exercise-induced bronchoconstriction: 3, 8-11
- Prescribe pre-exercise medication (e.g. inhaled short-acting β2-agonist). Note: caution is recommended against over use of inhaled β2-agonists, as this can lead to tolerance and it has been shown there is a correlation with asthma mortality in patients that have been prescribed more than 12 short acting reliever inhalers in the previous 12 months 12.
- Advise individuals to complete a warm-up that includes intermittent high-intensity exercise;
- Encourage individuals to exercise in warm humid environments (e.g. swimming pools) or, when exercising in cold weather, to cover their mouth with a scarf or use a face mask that warms and humidifies the air;
- Advise individuals to limit exposure to environmental triggers (e.g. air pollutants and allergens) when exercising.
Chronic Obstructive Pulmonary Disease (COPD)
Chronic obstructive pulmonary disease (COPD) results in irreversible damage to lung tissue and long-term inflammation of the airways, resulting in fixed airflow limitation. As COPD progresses, symptoms such as breathlessness and muscle fatigue make exercise an unpleasant experience, which, together with a sedentary lifestyle , leads to muscle deconditioning associated with reduced physical activity. This subsequently contributes to further decline in exercise capacity and perception of breathlessness. Thus, people with COPD get trapped in a vicious cycle of declining physical activity and increasing symptoms of breathlessness during exercise 1.
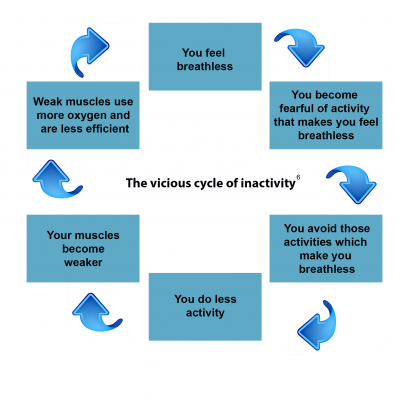
Pulmonary rehabilitation aims to break the vicious cycle of inactivity by enabling people with COPD to become more active under supervision and ultimately, less afraid of exerting themselves and getting out of breath. 1, 2. Pulmonary rehabilitation involves multidisciplinary programmes that are built around an exercise training intervention, patient education and relaxation techniques. The potential benefits of exercise training alone in people with COPD include: 3
- Improved health-related quality of life
- Increased psychological well-being
- Improved symptoms of breathlessness and limb discomfort
- Improved functional capacity
- Increased participation in everyday activities
- Lower morbidity with fewer hospital admissions
- Reduced length of stay following acute exacerbations
Physical inactivity is associated with a higher risk of hospital admissions and an increased risk of mortality in people with COPD, and contributes to disease progression and poor outcomes 4. Thus, NICE recommendations state that patients with a Medical Research Council (MRC) dyspnoea grade of 3-5 who are functionally limited by breathlessness should be referred for outpatient pulmonary rehabilitation 5. Further, the British Thoracic Society guidelines on pulmonary rehabilitation include COPD patients with a MRC dyspnoea grade of 2 who are functionally limited by breathlessness 6. However, physical activity should be considered an integral part of the clinical management of all people with COPD, irrespective of their MRC score. 1, 7.
NICE guidelines NG115 recommend: 5
- Make pulmonary rehabilitation available to all appropriate people with COPD, including people who have had a recent hospitalisation for an acute exacerbation;
- Offer pulmonary rehabilitation to all patients who view themselves as functionally disabled by COPD (usually MRC grade 3 and above);
- For pulmonary rehabilitation to be effective, and to improve adherence, they should be held at times that suit people, in buildings that are easy to get to and that have good access for people with disabilities;
- Pulmonary rehabilitation programmes should include multicomponent, multidisciplinary interventions that are tailored to the individual person’s needs. The rehabilitation process should incorporate a programme of physical training, disease education, and nutritional, psychological and behavioural intervention;
- Advise people of the benefits of pulmonary rehabilitation and the commitment needed to gain these.
Cystic Fibrosis
The progressive respiratory dysfunction associated with cystic fibrosis (CF) leads to fixed airways obstruction, abnormal ventilatory responses and subsequent breathlessness during exercise, which limits exercise capacity and the ability to perform activities of daily living. Low levels of physical activity contribute to disease progression in CF. 1 Further, lower levels of aerobic fitness are associated with a reduced life expectancy.2
Exercise is an important adjunct to treatment for patients with CF, irrespective of age and disease severity.3 While evidence for the efficacy of exercise training in CF is relatively limited,4 regular exercise and physical activity may provide a wide range of benefits, including:
- Increased exercise capacity
- Improved strength and endurance of the muscles of ventilation
- Reduced breathlessness
- Preserved pulmonary function
- Enhanced mucus clearance
NICE guidelines NG78 make the following recommendations:5
- Advise people with CF and their family members or carers (as appropriate) that regular exercise improves both lung function and overall fitness;
- Offer people with CF an individualised exercise programme, taking into account their capability and preferences;
- Regularly review exercise programmes to monitor the person's progress and ensure that the programme continues to be appropriate for their needs;
- Provide people with CF who are having inpatient care with:
- an assessment of their exercise capacity;
- the facilities and support to continue their exercise programme (as appropriate), taking into account the need to prevent cross-infection and local infection control guidelines.
Summary
Key messages:
- The benefits of exercise and incorporating exercise activities into a healthy lifestyle should be discussed with all patients with chronic respiratory diseases.
- Physical activity is well tolerated by people with stable asthma and should be recommended as supplementary therapy to medication.
- Physical activity and pulmonary rehabilitation should be considered an integral parst of the clinical management of all people with COPD
- Exercise training should be included in routine therapy for people with CF
Consider:
- Auditing and monitoring your patients to determine their physical activity levels
- Advising on the importance of this lifestyle approach for well-being
- Referring your patients to a pulmonary rehabilitation programme
- Consider high risk comorbidities which are common in patients with chronic lung disease
Signpost to additional support resources, such as found at The British Lung Foundation
Benefits for GP’s and Allied health professionals: Reduced admissions, outpatient appointments, drug costs and visits.
Acknowledgments: We would like to thank the following authors for contributing their help in making this chapter summary entitled; Physical Activity and Respiratory Disease: Pascale Kippelen and Lee Romer of The Department of Sport, Health and Exercise Sciences, Brunel University, London.
Now part of the RCGP clinical programme on physical activity and lifestyle
References: Can be found in Chapter 18
Updated February 2020 - Review December 2022




